Abstract
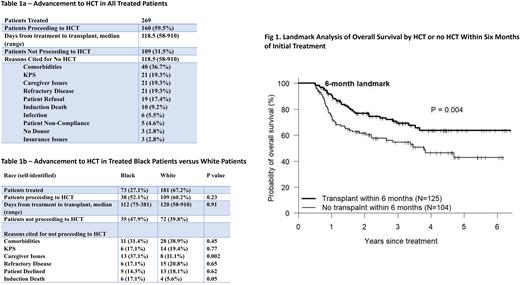
Hematopoietic cell transplantation (HCT) remains the most effective consolidation therapy in patients with non-favorable risk acute leukemia (AL) and MDS. However, prior studies have demonstrated that only a relatively small proportion of patients who may benefit, actually proceed to HCT. Lack of timely access to conventional matched donors, and delays in referral to transplant physicians have historically been important obstacles. At our center, AL care and HCT services are provided by the same physicians eliminating referral delays, and donor search/ transplant evaluation for all patients is commenced at program entry. Furthermore, HLA-haploidentical (haplo) donors have routinely been utilized since 2006. We hypothesized that these factors would increase the proportion of AL patients proceeding to HCT and decrease time to transplantation. We also analyzed other barriers to transplantation at our center, which includes a relatively high proportion of treated black patients. Methods: All patients aged <75 receiving initial therapy at our center for non-favorable risk AML, ALL or MDS between 2016 and 2021 were included. Non-favorable was defined as intermediate and poor-risk AML by NCCN criteria, NCCN poor-risk ALL patients (age <40) and all ALL patients aged >40), MDS EB-1 and EB-2 and CMML). Data were extracted from our institutional leukemia and transplant database where they had been prospectively entered. Results: Of 269 consecutive patients who received initial therapy at our center for non-favorable risk AL and MDS between Jan 2016 and Dec 2021, 160 (59.5%) proceeded to HCT at a median of 119d (range 58-910d) from initial therapy. For patients who did not proceed to HCT, most common cited reasons were: comorbidities (36.7%), poor KPS, lack of adequate caregiver support, refractory malignancy (19% each) and patient refusal (17.4%) (Table 1a). Lack of a donor and insurance issues were rarely a cause (3% each). For patients aged <60, 71% proceeded to HCT versus only 47.3% of patients aged 60-75 (p<0.001). Comorbidities (15% vs 49.3%, p<0.001) and KPS (10% vs 24.6%, p=0.06) were less common as reasons for not proceeding to transplant in patients aged <60 vs 60-75, whereas lack of caregiver support was more common in patients aged <60 (30% vs 13%, p=0.031). Of 73 black patients treated, 52.1% received HCT vs 60.2% of 181 treated white patients (p=0.23)(Table 1b). However, lack of caregiver support (37.1% vs 11.1%, p=0.002) and induction death (17.1% vs 5.6% p=0.05), were more common reasons in black patients for no HCT. AML and ALL patients had a similar likelihood of proceeding to HCT (57.6% vs 61.6%) but refractory disease was more common in AML (25.6% vs 3.6%, p=0.012) as a reason for no HCT. For AML patients, a higher proportion of patients with intermediate risk disease vs poor-risk disease proceeded to HCT (71.7% vs 50.8%, p=0.007). On logistic regression analysis, age (OR 1.46 per 10 yr increment, p<0.001) and NCCN poor-risk (OR 1.83, p=0.032) were significant factors for failure to proceed to HCT. Characteristics of patients who proceeded to HCT were: median age 55 (18-75); 49% male; race- white 68%, black 24%, Asian 7%; donor -haplo 41%, MRD 29%, MUD 22%, auto 8%; cell source- PBSC 93%, BM 4%, CBU 3%; disease status - CR1 83%, other 17%. Median time from initial treatment to HCT were shorter for AML vs ALL (114 vs 136 d, p=0.002), MRD and haplo vs MUD - 113d each vs 148 d, p=0.011) but were similar for black vs white patients (112d vs 120d, p=0.91). In a landmark analysis, patients receiving HCT within 6 months since starting treatment had significantly better OS than those without HCT within 6 months (Fig 1). On multivariable Cox analysis assessing transplant as a time-dependent covariate, adjusting for patient age and year of treatment, HCT was of significant benefit compared to no-HCT for overall survival (HR 0.59, p=0.012) and disease-free survival (HR 0.64, p=0.025). Conclusions: Our data suggest that in a modern cohort treated within an integrated AL/HCT program incorporating routine use of haplo donors, up to 60% of all treated patients (71% for age <60) with non-favorable risk AL and MDS can proceed to HCT in a median of 118 d from initial treatment. This approach results in no significant difference in proportion transplanted or time to HCT between black and white patients but caregiver support maybe a greater barrier in black patients. HCT is associated with a significant survival benefit.
Disclosures
Solh:ADC Therapeutics: Research Funding; Partner Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal